New Maternal Mortality Data and Analysis Published by CDC and Commonwealth Fund
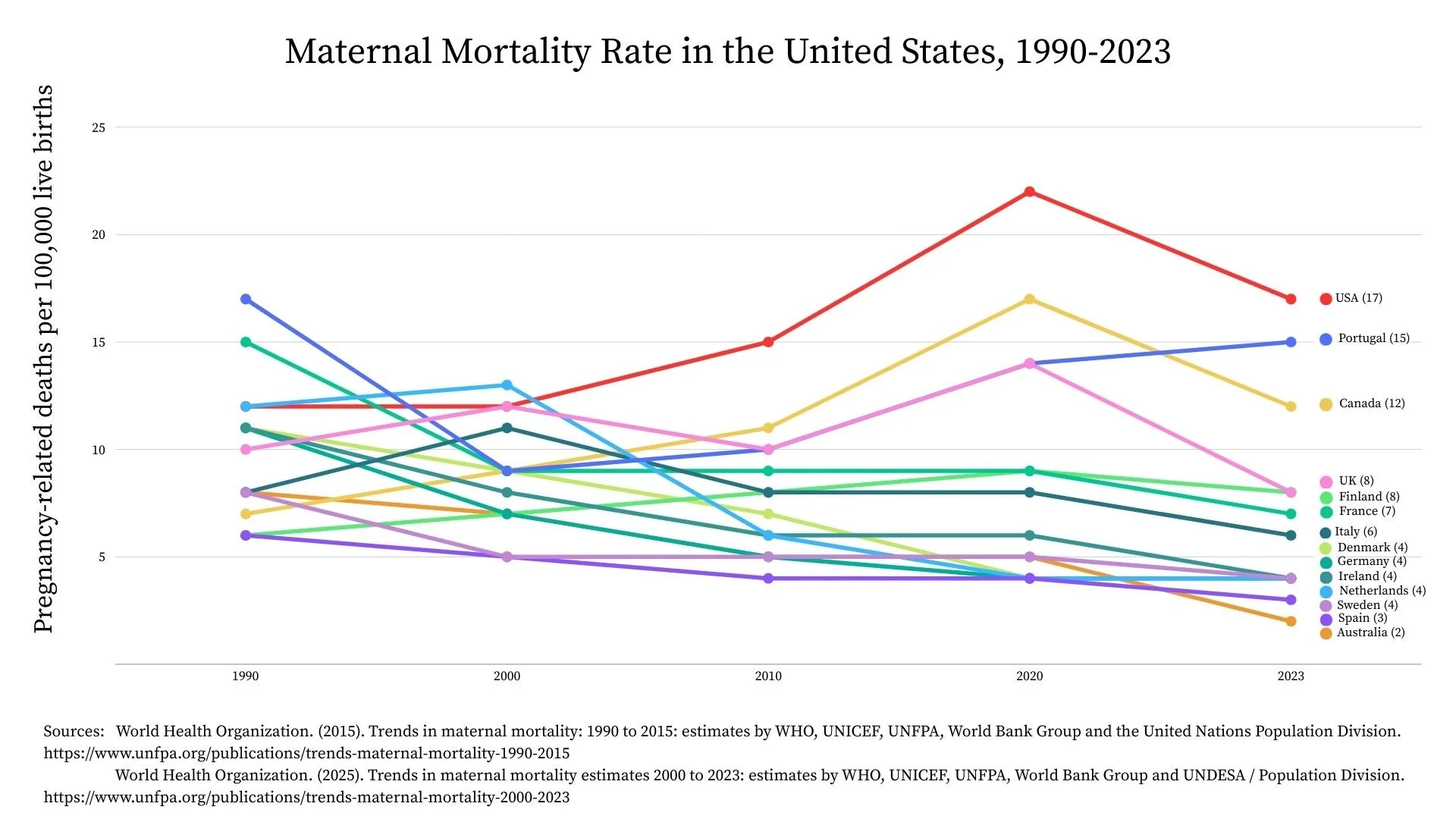
On August 22, 2025, the Centers for Disease Control and Prevention (CDC) published new maternal mortality data from 2021. The U.S. continues to have the highest maternal mortality rate of all other high income nations.
Key Takeaways
908 women died during pregnancy or the year following pregnancy in 2021. [NOTE: This is a spike in maternal deaths due to COVID-19; maternal mortality rates have returned to pre-pandemic levels (approximately 700 maternal deaths each year).]
33% of maternal deaths were due to infection (COVID-19), which was the leading cause of death.
23% of maternal deaths were due to underlying mental health conditions. [NOTE: This is the same rate reported by the CDC for maternal deaths in the four preceding years.]
31% of deaths with underlying mental health conditions were identified as suicides.
87% of pregnancy-related deaths were deemed to be preventable.
About this Data
The CDC compiles and analyzes maternal mortality data from Maternal Mortality Review Committees (MMRCs), which are multidisciplinary committees that convene at the state or local level to comprehensively review deaths during or within a year of pregnancy (pregnancy-associated deaths).
With each reporting period, additional MMRCs are submitting data from their states. This data for 2021 comes from 46 states; reporting for 2020 included data from 38 states; reporting for 2017-2019 included data from 36 states; and reporting for 2008-2017 included data from just 14 states.
MMRCs provide the most robust data about pregnancy-associated deaths as they include data from the entire perinatal period (during pregnancy and the full year following pregnancy) and also include information about deaths due to suicide, overdose, and homicide.
Causes of Death Differ for Racial and Ethnic Groups
It is important to note that causes of death differ for specific racial and ethnic groups. The CDC continues to refine data collected about maternal deaths and now disaggregates data as follows:
American Indian or Alaska Native (AI/AN)
Hispanic
non-Hispanic Asian
non-Hispanic Black
non-Hispanic multiple races
non-Hispanic Native Hawaiian or Pacific Islander
non-Hispanic other
non-Hispanic white
Circumstances Surrounding Death
There are four "circumstances surrounding a pregnancy-related death" that can be documented by MMRCs using standard checkboxes. These circumstances were identified as contributing to the death, and not just whether the circumstance was present.
OBESITY contributed to 29% of deaths. The committee may determine that obesity contributed to the death when the condition directly compromised a women's health or health care. For example, obesity complicated ventilation options for a pregnant woman with the flu.
DISCRIMINATION likely contributed to 32% of deaths. Discrimination is defined as treating someone less or more favorably based on the group, class, or category they belong to. For example, dismissing symptoms of abdominal pain described by a woman with a history of substance use disorder led to a delay in diagnosis and care for ruptured ectopic pregnancy.
MENTAL HEALTH CONDITIONS contributed to 22% of deaths. The committee may determine that a mental health condition is a circumstance that contributed to the death when the condition directly compromised a women's health or health care. For example, a mental health condition impacted her ability to manage type 2 diabetes.
SUBSTANCE USE DISORDER contributed to 24% of deaths. The committee may determine that substance use disorder is a circumstance that contributed to the death when the disorder directly compromised a women's health or health care. For example, acute methamphetamine intoxication made preeclampsia worse, or she was more vulnerable to infections or medical conditions.
Updated Analysis on Maternal Mortality in the U.S. by The Commonwealth Fund
The Commonwealth Fund has been providing excellent analysis of maternal mortality information since 2020, with most recent updates published in July 2025.
The Impact of COVID-19 on Maternal Mortality
This new report from The Commonwealth Fund highlighted some important data regarding the impact of the pandemic on maternal mortality, which aligns with the CDC data above:
The pandemic exacerbated existing racial disparities in pregnancy-related deaths.
The impact of the pandemic on pregnancy-related deaths peaked in 2021.
Hispanic women who died of pregnancy-related causes in 2020 were 5-16 times more likely to have COVID than non-Hispanic white women.
Other Key Takeaways from the Report
There are significant racial and ethnic disparities in the underlying causes of pregnancy-related deaths.
The risk of pregnancy-related death increases steadily with age.
There were wide interstate differences in pregnancy-related deaths.
Mortality ratios in rural areas were over 50 percent higher than in large urban areas.
In summary, maternal health cannot be viewed separately from the overall health of women and infants, from social needs, or from the impact of disparate access to high-quality and accessible care.
STAY IN TOUCH